The Ravin Technique–The injured ligament treatment
Prolotherapy is a treatment for lax ligaments that is done by a physician. The goal is to stimulate the growth of new collagen the building blocks of ligament tissue.
There are currently five ways that physicians have to accomplish this goal. All of these methods will work better in dense connective tissue such as ligaments.
They are:
- Creating an acute inflammation by causing tissue to repair using concentrated sugar water.
- Injecting an irritating material such as pumice into the ligament to stimulate the resident fibroblasts to produce collagen.
- Injecting growth factors into the ligament tissue stimulate the resident fibroblasts to produce collagen.
- Injecting platelets into the ligament stimulate the resident fibroblasts to produce collagen.
- Injecting stem cells into the ligaments.
Under which conditions can prolotherapy complement the natural wound-healing tissue process in tightening a lax ligament?
- Ligament strain caused by poor posture or poor technique while doing any activity or practicing any sport.
- Prevention of ligament healing caused by a non-steroidal anti-inflammatory drug (NSAID) such as aspirin or ibuprofen taken for pain relief after an injury. NSAIDs inhibit some of the early chemical reactions in the inflammatory phase, particularly the production of prostaglandin E2. A lower prostaglandin level means fewer macrophages attract to a wound.
- Decrease in collagen production in the inflammation and granulation phases of wound healing and tissue repair caused by inadequate protein intake or protein that is redirected to repair vital organs after a major accident or trauma.
- Decrease in the blood supply to the injured tissue and in the quality of the repair process caused by smoking.
These methods will work on parts of injured tendons but, in general, tendinosis repair is achieved by a different process that does not respond as well to the proliferants below. Tendinosis is most often the direct result of ligamentous laxity at the adjacent joint and needs to be treated first. Treatment of tendinosis besides injections to the ligament also requires modification of the activity that created the injury in the first place, such as the duration, intensity, style, posture and equipment.
Types of Proliferants
Concentrated sugar water
Concentrated sugar water is water with enough dextrose (a sugar) to make it hyper-osmotic enough to cause tissue damage. It does this by literally sucking the water out of the cells that it comes into contract with. This leads to death of the affected cell and the contents are spilled into the tissue. This causes a direct injury to the ligament and some of the adjacent tissues. The injury stimulates the body’s natural ability to heal wounds and repair injured tissues such as ligaments. In this injured region small blood clots form and the body begins the process of repairing the ligament using the process detailed below.
The highlighted material is what is website now. We can leave it here or link to it.
One of the most common ways prolotherapy works is by stimulating the body’s natural ability to heal wounds and repair injured tissues such as ligaments and tendons. A ligament is like a cable or twine, which, when stretched too far and too fast, begins to fray. In this frayed region, small blood clots form and the body begins the process of repairing the ligament.
All tissues in the body that are wounded or need to be repaired go through three phases:
- Inflammation
- Granulation
- Remodeling
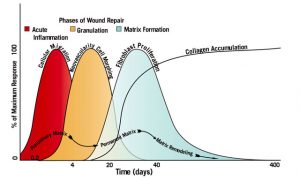
Although this discussion concerns the ligaments, the deepest of the soft tissue structures, the skin, heals in almost the same manner. Small skin cuts heal in much the same way as deeper structures. The main difference is that ligaments and other deep tissues do so without scarring. Figure 1 shows the phases of wound healing.
Inflammation is the initial phase of wound healing. For the first 100 hours after an injury, a blood clot forms, laying the groundwork for many cellular and chemical activities. The blood clot traps platelets, small particles in the blood that contain many growth factors, that guide this phase. The blood clot also captures and attracts many other cells. Some of these cells kill the bacteria that have entered the wound (leukocytes), others clean up the dead tissue in the wound (neutrophils), and still others become involved in the repair process (macrophages).
Some of the chemical reactions produce substances, in particular, prostaglandinΕ2 that cause irritation of the pain fibers. Other chemicals released by the injured tissue and the platelets not only send signals to the healthy cells adjacent to the wound and the incoming macrophages specifying which ligament is injured, but also direct these cells to download the repair information from their genes. These cells multiply with the “genetic blueprint” for the repair. Once the chemical reactions are finished and the cells have obtained the necessary genetic information, the inflammation phase ends.
Approximately 100 hours after the injury, the granulation phase begins during which many cells multiply and change shape. Some macrophages turn into fibroblasts, which make collagen. Existing blood vessels are stimulated to make new ones that supply the new tissue with oxygen and nutrients. As a coordinated unit, the fibroblasts and blood vessels move into the wound, creating the granular appearance for which this phase is named. This cycle of creating collagen, the raw materials of a ligament, continues for the next 3 to 5 weeks. As this phase ends, the collagen begins to reorganize into the matrix of the new ligament.
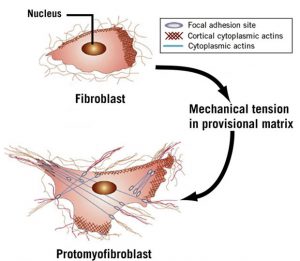
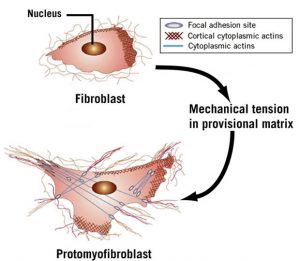
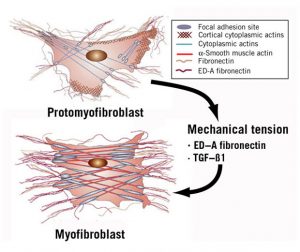
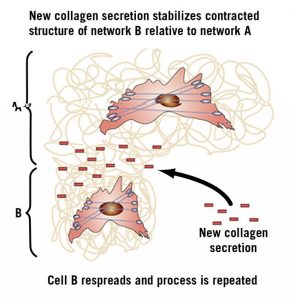
The remodeling phase, which is more difficult to observe, takes about 12 weeks. During remodeling, the superficial blood clot drops off the skin. The wounded area underneath is still red and slightly raised but usually not tender. In an injured ligament, the collagen resembles gelatin more than a ligament. Within this disorganized collagen, a few fibroblasts, or the cells that make collagen, evolve into a different kind of cell that begins to produce muscle contractile fibers in response to stress or the constant tugging of the new tissue by movement. These cells with powerful contractile fibers are called myofibroblasts. (See Figures 2 and 3)
Myofibroblasts begin attaching to some of the disorganized collagen, contracting and pulling the adjacent collagen into a tighter, more compact matrix. In the area of the compacted matrix, new collagen cements the fibers in their shortened positions. This process continues until all of the myofibroblasts are shielded from the stress by the new ligament tissue; then they disappear. (See Figures 4 and 5) At the end of the remodeling phase, the gelatin has been organized into a new ligament that has been repaired to its original strength and length and is indistinguishable from the original. In other words, there is no scar tissue. This process gives humans and animals the resources to repair minor injuries in such a way that survivability is not affected. (1)
Under which conditions can prolotherapy complement the natural wound-healing and tissue process in tightening a lax ligament?
Concentrated sugar water is the most widely used proliferant because:
- It is safe.
- It is water soluble.
- It is easy to use.
- It is readily available.
- The amount of dextrose added to the water can be easily varied.
- It is cost efficient.
- There is a lot of supporting research about its use in musculoskeletal medicine. (2)
Comment: I to not use this proliferant very often. I have found that it is slightly more painful when used in concentrations high enough to get good results when compared to the other proliferants I have available.
Growth Factors and Hormones
The second mechanism that can increase the density of connective tissue like ligaments and fascia is by using growth factors to stimulate the fibroblasts that reside in the ligament tissue to produce more collagen. Testosterone has been used for the purpose enhancing overall body strength and for bodybuilding since the 1950s. (3)
How testosterone promotes muscle and ligament growth was scientifically defined in the 1950s. (4) The scientists at the time unraveled this process. They observed hormones attached to receptors on the cell wall and were transported into the nucleus. Once in the nucleus the specific genes that define the make up of molecules of muscles and ligaments were stimulated and with testosterone the final effect was larger and stronger muscles and ligaments.
This method of hormone action was the standard explanation of how hormones worked and not just for testosterone but hormones in general. This mechanism is defined as the ‘genetic effects’ of hormones. The ‘genetic effects‘ model explained the long time delay of minutes to hours between when the hormone was introduced into the body and when some effect could be identified. Research over the next thirty years reinforced the power of this explanation and the standard explanation for hormones until the 2000s.
Beginning in the later 2000s evidence that some hormones and in particular those related to growth could be demonstrated to work within seconds and that some cells from the brain, heart and muscles created testosterone themselves within seconds. These findings suggested that there was another signaling system that bypassed the nucleus. This second mechanism was called ‘non-genetic effects‘ because it was clear that they were effecting some tissue too fast for the genes to be involved. (5)
Recent research as well as clinical observations has established that testosterone and growth hormone are made and secreted by many different types of cells including the fibroblasts and myoblasts that reside in the ligaments and tendons.(6) It has been shown that muscle and ligament, during strenuous bursts of activity, make their own growth hormone(GH) and insulin-like-growth factor (IGF-1). This leads to the local increase in number and size muscle and ligament fibers.(7) The injection of testosterone and GH in prolotherapy into loose ligaments uses the ‘non-genetic effects‘ of these two hormones to stimulate the body to make more ligament. (8)
The hormones testosterone, hGh and the peptide IGF-1 have over the last 10 years been documented to be safe, easy to use, cause no systematic effects with the doses used. (9)
Comment: This is my favorite proliferant for ligaments that are articular or a part of the joint capsule and they work as well as or better than sugar water or PRP and are less expensive and easier to use.
These include:
- Shoulders
- Elbows
- Wrist, hand and thumb and fingers
- TMJ
- Hips
- Knees
- Ankles
- Feet
- Tendinosis adjacent to joints
- Other joints not mentioned
Platelet Rich Plasma (PRP)
Platelets are a component of blood whose function along with the coagulation factors is to stop bleeding by clumping and clotting blood vessel injuries and create a temporary matrix that holds the wound together by forming a clot. The platelets clump together to plug the leaking vessels and the clotting factors create a fibrin clot that forms a matrix that fills in the injury site if it is not to big. (10)
The platelets also contain small particles called ‘alpha granules’. These contain multiple growth factors such as PDGF (platelet derived growth factor), IGF-1, transforming growth factor beta (TGFβ) and vascular endothelial growth factor (VEGF). The IFG-1 is a key factor in many aspects of cell growth and function and, in particular, signaling the creation of collagen. It is the high concentration of these growth factors in PRP that is stimulating the growth of collagen through ‘non-genetic effects‘ of hormones.
There is a little research that PRP is effective in treating some musculoskeletal problems. It does require having the blood drawn and them spun down to get the platelets, which add extra time and cost to the treatment. The size of the treatment is also limited by the small amount of platelets that can be harvested at any one time.
Comment: I do not have a PRP machine as I feel that the hormones are easier, safer, less expensive and yield better outcomes than PRP. I occasionally feel that PRP might be a better choice than the growth factors and hormones and I have several local colleagues who I can refer the patient to for that kind of treatment if I feel that it would be beneficial.
Pumice
The third way to stimulate the growth of new collagen tissue is the injection of a substance that irritates the fibroblasts that are responsible for maintaining the ligament. The material used to do this is called pumice. Pumice is just a specific type of lava rock. Lava is a type of glass that is non-antigenic and chemically inert. The pumice that is used by physicians is the same that is used by the dentist to polish crowns and teeth after cleaning. It is these small particles of glass that you cannot feel with the tongue but make the ‘crunchy’ noise in your mouth as you walk out of the dentist’s office. There is another way to visualize pumice. The dust cloud in New York City that drifted down the streets adjacent to the World Trade Center buildings as they collapsed was pumice. This cloud was created by the glass sidings of the buildings as they were literally pulverized into glass dust, which was so small it got to the most remote parts of the lungs of the first responders to the tragedy.
Pumice acts on the resident fibroblasts of the ligament. Fibroblasts are the cells that are responsible for maintaining the integrity of the connective tissues of the body and in particular the ligaments and fascia. The pumice particles, when injected into the ligament, cause irritation of these fibroblasts that respond by secreting collagen molecules that are then remodeled into ligament fibrils. As the fibrils shorten the irritation of the fibroblasts decreases until they are no longer irritated. These changes eventually shorten the whole ligament until the instability and pain from the ligament is corrected. The fibroblast achieves this by using the same pathways as illustrated in the inflammation section. This treatment is the most durable because the pumice, once working, continues to work again if the ligament is over used or reinjured.
In the early 1900s French doctors primarily used Pumice to treat hernias. There are no articles and only a few mentions of its uses in English medical literature and those are hard to find. Earl Gedney was one of the first physicians to do prolotherapy and his knowledge of pumice was probably because of his interest in treating hernias in the late 1930s. His enthusiasm for its use to treat the low back pain of his coalmining patients in eastern Ohio lead to it being used much more extensively in the 1940s and 1950s by many physicians.
Its current use is limited to just those prolotherapists who feel comfortable with their diagnostic and injection skills. The use of pumice is considered an advanced injection technique because once injected there’s no getting it out. Pumice seems to work best in dense connective tissue like big ligaments and dense fascia. Its major advantage is that is can decrease the number of needed injections at any location by about 30 to 40 percent.
Comment: This is my go-to proliferant for most extra articular ligaments and includes these ligaments:
- Sacroiliac
- Coracoclavicular and sternoclavicular
- Forearm and ankle interosseous
- Tendinosis, which has been resistant to other proliferants and rehabilitation.
Stem Cells
At this time, the use of stem cells to stimulate ligament growth or repair has only some animal studies and some clinical evidence that it works in some musculoskeletal situations. There is little clinical evidence that it works better that any of the previously discussed proliferants. The future of stem cells in musculoskeletal medicine looks promising but there are many barriers to its broad clinical use, the least of which is the extremely high cost.
References:
(1) Shaw TJ, Martin P. Wound repair at a glance Journal of Cell Science 2009;122:3209-3213 doi:10.1242/jcs.031187
(2) Hauser RA, Lackner JB, Steilen-Matias D, David K. Harris DK A Systematic Review of Dextrose Prolotherapy for Chronic Musculoskeletal Pain Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders 2016:9 139–159 doi: 10.4137/CMAMD.S39160.
(3) Tyagi V, Scordo M, Yoon RS, Liporace FA, Greene LW Revisiting the Role of Testosterone: Are We Missing Something? Rev Urol2017;19(1):16-24 doi: 10.3909/riu0716
(4) Hoberman JM, Vesalis CE The History of Synthetic Testosterone Scientific Am1995;2:76-81
(5) Foradori CD, Weiser MJ, Handa RJ. Non-genomic Actions of Androgens2008 May ; 29(2): 169–181. doi:10.1016/j.yfrne.2007.10.005.
(6) Cornil CA, Ball GF, Balthazart J Functional significance of the rapid regulation of brain estrogens: Where do the estrogens come from? Brain Res 2006 December 18; 1126(1): 2–26. doi:10.1016/j.brainres.2006.07.098.
(7) Vestergaard P, Jørgensen JO, Hansen M. et.al. Local administration of growth hormone stimulates tendon collagen synthesis in elderly men. J Appl Physiol 113: 1432–1438, 2012.
(8) Boesen AP, Dideriksen K, Magnusson SP, , Kjaer M, Langberg H. Effect of growth hormone on aging connective tissue in muscle and tendon: gene expression, morphology, and function following immobilization and rehabilitation. J Appl Physiol 116: 192–203, 2014.
(9) Dubick M, Ravin TH, Michel Y, Morresette DC. Use of localized human growth hormone and testosterone injections in addition to manual therapy and exercise for lower back pain: a case series with 12-month follow-up Journal of Pain Research 2015:8;295-302
(10) Wikepedia. Platelet Rich Plasma Nov 11, 2017.